Cleanliness is next to production standardization requirements for medical device manufacturers (as the old saying goes). Devices built to be inserted within the human body understandably need to meet the highest cleanliness standards. Companies in this industry have already known what many of us are learning for the first time: clean isn’t always clean, and a visual once-over doesn’t cut it when trying to determine if there are invisible contaminants on a surface.
There can be a couple of big buckets that cleanliness concerns might fall into. One is sterilization, being able to keep product surfaces (especially those that come into contact with patients or end users) free of biological contamination. The other is cleanliness for functionality, which is also related to safety concerns but has different processes and controls during production than disinfection procedures often involve.
Functional cleanliness can also be called chemical cleanliness. A surface that is chemically contaminated has substances present at the top few molecular layers that make bonding to the material difficult or, at the very least, will result in a weak and unreliable bond. For medical devices, the uncertainty of this magnitude is unacceptable. Every device must function as designed and expected every single time.
Optimize the power of next-gen connectivity with data & surface intelligence.
A lot of certainty is built into the design of the manufacturing processes to build these devices, and the validation of these processes helps to ensure that they are on track to create consistent, high-reliability devices.
There’s more than one way to clean or prepare a surface, and choosing the most effective one has a lot to do with the type of material and the type of bonding (i.e. gluing with an epoxy, sealing with FIPG, coating or painting metal, bonding polymers, etc.).
For this article, we’re going to hone in on aqueous and chemical wash methods primarily used to clean metal components before bonding or coating. When performing these tasks within a medical device assembly process, the dual pressures of cleanliness (biological and chemical) are equally vital to yielding the safest and most effective medical devices possible.
FDA QSR 820.75 Standards for Process Validation
The FDA has prescribed requirements for how medical device manufacturers can design and build a process that invariably generates in-spec products. Within these requirements, there can be a range of acceptability for all inputs, but how can a manufacturer be certain all of the cleaning, coating, bonding, and assembly operations are within this range?
To learn more cleaning processes that results in the highest quality, and most safe medical devices possible, download our eBook: Predictable Adhesion in Manufacturing Through Process Verification
The QSR 820.75 mandates monitoring at a determined interval and frequency (based on statistical analysis), but continuous monitoring is preferred. You should periodically evaluate the monitoring interval and frequency as well—especially if you change the process or uncover a deviation from the specification.
Types of Biological Contamination
Microbial contamination comes in a few forms, and each threat has assays and tests to ensure they are neutralized during production. At several points throughout production, microbes and bacterial and chemical contamination can interact with the surfaces of the devices, rendering them too contaminated for use and/or too contaminated to be reliably assembled.
Biological contaminants that make devices unsafe for use will typically have little to no impact on the bondability of a part typically because these substances are unlikely to be in a film on the surface and are likely to be absorbed into a coating or adhesive applied to the surface. A biologically clean surface is one that is free of pathogens and viral microbes. This is distinct from chemical cleanliness in that a surface that has been cleaned properly for excellent adhesion may not necessarily be biologically clean. When cleaning a surface to sterilize it, a disinfecting cleaner may be used to cover the surface with an antibacterial liquid (for instance, one containing bleach) and let it sit there to kill the microbes that may be present on the surface.
Wash processes in manufacturing (much like when we wash our hands - removing germs from our skin through friction and a surfactant, then sending them down the drain) can prevent microbial contamination. These processes can serve the dual purpose of cleaning surfaces to create reliable bonds and to ensure they won’t cause infection or disease when used.
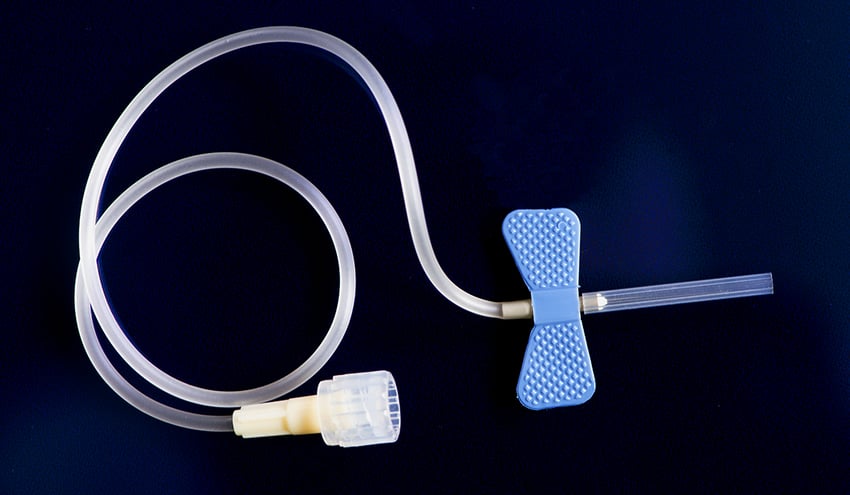
The class of a medical device is one determinant of what level of testing and validation is required. The classification of medical devices is based on the nature of contact with a patient. Re-usable examination tools with incidental patient contact might be tested for function and, possibly, bioburden (1). Implantable medical devices with years of intimate, internal patient contact might also be tested for endotoxins (2), cytotoxicity (3), sterility, as well as functionality.
- Bioburden is the amount of viable microbes on the surface of a device, and this amount must be lower than the limits outlined for sterilization.
- Endotoxins are bacterial contaminants that are released when a cell disintegrates. Any time a medical device comes into contact with water during a manufacturing process, there is a possibility of endotoxin contamination.
- Cytotoxicity refers to leachable components within medical devices that can damage or kill human cells and prove to be toxic to patients.
There are other tests that check for safety that have to do with coatings and surfaces, like Hemocompatibility testing of blood-contacting medical devices. This is one of the most important criteria for the successful clinical application of these sorts of devices, and the hydrophobic or hydrophilic coating must be uniformly applied to the surface, which cannot be done if the surface isn’t properly cleaned for chemical contamination.
Parts Washing Technologies for Metal Components
Metal components in medical devices can be particularly difficult to clean. They are often unusual shapes, with small crevices and blindspots that need to be cleaned, and they often will be encapsulated with a polymer coating that needs to conform completely and perfectly around the metal.
A device that is designed to exist within a human body for long stretches of time may have a titanium base that electronic components will adhere to. Then the whole package will be encapsulated with a highly lubricious, non-reactive polymer. It is critical that the electronics are bonded strongly and securely to the titanium and that the polymer can adhere to the device.
For this article, however, we’re just focusing on cleaning the metal, but if you’re interested in adhesion for difficult to bond to polymers, check out this resource.
The machines tasked with cleaning metal parts have moved from what amounts to large-scale dishwashers to highly advanced ultrasonic aqueous baths and vapor degreasing systems. Ultrasonic parts washers are immersive tanks that pulse the solution or water a component is submerged in using high-frequency sound waves to release contaminants from the surface of the part. Vapor degreasing systems are also immersive, but they use an evaporated solvent to dissolve oils, greases, and fluxes from mechanical and electronic parts.
Vapor degreasers are becoming more common as they are touted as being more economical and safer for the environment. The latter point isn’t necessarily accurate since many of these machines are being used with halogenated solvents, which are being found to be harmful to patients, manufacturing employees, and the environment. The EPA is putting restrictions on their use and has already banned them from inclusion in consumer products such as paint removers.
These changes are always good to stay aware of because changing the solvents used can have a major impact on the wash's efficacy.
To control washing systems that include a spray mechanism, many manufacturers will very precisely dial in their nozzles to ensure the angles are the most efficient (cover the most surface area), the aggressiveness of the spray is highly controlled, and that each nozzle doesn’t have gunk buildup on the holes leading to errant spraying or improper pressure.
One thing manufacturers using aqueous baths often overlook is the dangers of a recirculated wash fluid. This can be an extremely cost-efficient wash method but, if left unchecked, could contaminate parts as they are introduced to the bath. Manufacturers will often test for bioburden at these stages, which the solvents in the baths will usually take care of, but if they are not testing the chemical state of the surfaces of parts that come out of these washers, they may see issues downstream when they need to bond to these components.
Struggling with adhesion failures? Been there. Solved that.
Testing for adhesion-resistant contamination before and after washes will resolve this issue and flag when recirculated fluids are no longer producing coating-ready surfaces.
Similarly, vapor degreasers are a version of a solvent bath that functions on the principle of reusing the same solvent over and over. In this method, the temperature of a solvent bath is raised by a heating coil, and the vapor emanating from the solvent rises into a chamber that is holding the part being treated. The solvent vapor removes the contaminant by condensing on and then dripping off the surface of the part, breaking up and removing contaminants. Often the solvent is recovered and reused. This process needs to be closely monitored to ensure that the solvent is properly distilled and contaminant free when reused. The solvent also needs to be suitable for the material and entirely rinsed off before adhering to the part.
Chemical contamination testing needs to be done in a quantifiable manner using a technique that is reliable and repeatable so it can be used to fully verify the products and be documented to satisfy FDA regulations.
Built-in Controls Might not Test for Contamination Loading
Testing for various kinds of contamination takes place with these baths, but many of them are only inspecting for the kinds of biological organisms mentioned earlier. There are also sensors in the baths to control parameters such as temperature, fluid volume, ultrasonic pulses, etc. They are not necessarily testing for contamination loading in the wash solution. As contaminants are removed from the surfaces of metals, they go directly into the fluid the parts are sitting in, and without proper monitoring, these contaminants could transfer to subsequent parts.
A useful rubric for what elements need to be controlled in a cleaning operation is TACT:
Temperature
Many wash solutions can be used at ambient temperatures, but some still require some heating element. If the solution is too hot, it could warp some materials and will have an effect on the drying time.
Agitation
Controls the type of movement of the solution in the wash system. The type of agitation is a predominant basis for what kind of fluids are used. Some spray systems need a low-foaming detergent, and the type of solution in an ultrasonic bath and vapor degreaser are different because of the type of agitation employed.
Concentration
Controlling the ratio of detergent concentrate to water can have an effect on parts forming rust or how effective the rinse cycle is afterward.
Time
Time covers the entire wash process; pre-wash, number of wash stages, number of rinse stages, and drying time. To remove all biological and chemical contaminants, solvents need time to kill microbes or remove residues fully.
Parts washing and ultrasonic cleaning can be effective in ensuring parts are chemically clean, but the effectiveness of the cleaning process is influenced by many factors:
- Because parts can enter the washing process in various states of cleanliness, the effectiveness of the washing process may not be sufficient for excessively soiled or contaminated parts.
- The quality of the cleaning solutions degrades as parts are cleaned. If the cleaning solutions are not monitored and changed as appropriate, the cleaning process loses its effectiveness.
- Washing systems that include sprayers have a greater tendency to not clean uniformly depending on where the sprayer is actually directed at on the part being washed. Sometimes this is adequate, but for applications requiring high-precision cleaning, a spray wash may be too variable in its consistency.
- Parts entering the cleaning process are not always at the same baseline of cleaning, and this is seldom recognized or compensated for.
- Contaminants can be introduced after the washing process, and the surface quality of parts degrades over time as they are stored in inventory.
To ensure all of these factors are tested and accounted for, make sure you are inspecting the chemical state of your surfaces throughout the entire cleaning and assembly process. Technologies exist that make this kind of product verification easy and fast and are designed to be used directly on real parts in production settings without biologically contaminating the surfaces.
To learn more about verifying the effectiveness of your cleaning process by measuring surface quality as it relates to adhesion, download our eBook about verification techniques. The information in this book will put you on the right path to a predictable coating and adhesion process that results in the highest quality and most safe medical devices possible. Download it now: How to Streamline Process Design to Production for Medical