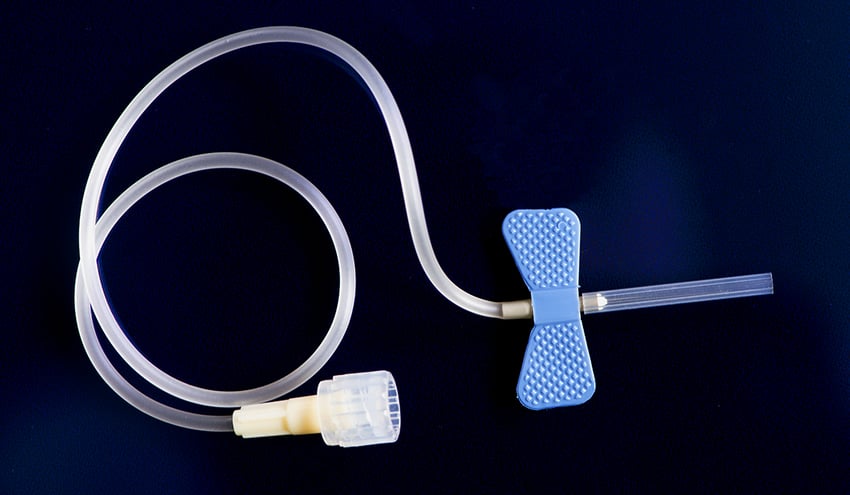
Comfort is more than just a nice thing to hope for when it comes to medical devices like tubing, catheters and stents that are implanted into the human body. Comfort, in this instance, refers to the absence of pain. Having a piece of plastic or metal inserted into your body is never going to feel like a warm blanket wrapping around you or like sliding slowly into a hot tub, but it is possible to make sure that these vital instruments are doing their job while not causing any damage or pain in the process.
The role of lubricious, hydrophilic coatings on the surface of implantable medical devices is to provide this pain-reducing service.
The FDA qualifies the function of coatings in this way:
“Medical devices such as intravascular catheters, guidewires, balloon angioplasty catheters, delivery sheaths, and implant delivery systems are commonly used during minimally invasive diagnostic and therapeutic procedures in the cerebrovascular, cardiovascular, and peripheral vascular systems. These devices often have hydrophilic and/or hydrophobic lubricious coatings (e.g., polyvinylpyrrolidone (PVP), polytetrafluoroethylene (How to Know if Hydrophilic Coatings on Medical Devices Provide the Necessary Comfort for Patients), silicone) to reduce friction between devices, and between the device(s) and blood vessels. It is commonly believed that these coatings may offer physicians greater maneuverability and may result in less trauma to blood vessels for patients.”
Manufacturers of these devices (i.e. the ones who apply the coatings) are far removed from the actual use of the medical products in the surgery rooms and hospitals. But they are looking for better ways to control the performance of the coatings so that everyone involved can be completely assured that:
- The coatings are sufficiently applied and uniformly present on the surface
- The coatings will effectively allow blood to wick over the implanted device or tubing
- The coatings will have a long lifespan that will not diminish the device’s effectiveness or reduce the comfort of the patient while in use
- All performance concerns that fall under the standards required by oversight groups are met
We’ll look at tests used to create certainty and predictability in the manufacturing process of these devices when it comes to the presence of coatings as well as their performance when it comes to patient comfort and safety.
Optimize the power of next-gen connectivity with data & surface intelligence.
Performance Testing of Medical Devices
As a part of testing regimens medical devices go through to document their reliability, you have testing for:
- Biocompatibility of materials the devices are made of
- Sterility of any materials that will make contact with the patient for any duration of time
- Pyrogenicity, which looks at the endotoxin and other pyrogen levels on material surfaces that can cause infections in the patient
- Packaging and storage shelf life to ensure that sealed medical devices will stay sterile and usable inside their packaging until the time they are deemed to be expired
- Non-clinical testing of things like the tensile strength of joints, size verification, and kink resistance is needed to make sure guidewires don’t bend and kink when being used.
That last one -- non-clinical performance testing or non-clinical bench testing -- is a testing process that scrutinizes devices to determine how well they’ll live up to the demands placed on them in actual use.
Any device that will be implanted into a human body should have a documented method of ensuring that it will not cause infection, will not cause the patient undue discomfort or pain, and will not become prematurely useless by corroding or falling apart.
Part of ensuring that medical devices meet requirements is to do coating integrity and lubricity testing, which directly examines the application of coatings, the strength of the bond to the surface, and the hydrophilicity of the coating.
Each aspect of non-clinical bench testing has a significant impact on the effectiveness of the device, but the consequences of coating failures are truly catastrophic.
The FDA lays it out like this: “Coating separation (i.e., peeling, flaking, shedding delamination and/or sloughing off) or degradation may adversely impact clinical performance (e.g., result in inflammation at the access site, pulmonary embolization, pulmonary infarct, myocardial embolization, myocardial infarct, embolic stroke, cerebral infarct, tissue necrosis, or death).”
It’s extremely important to control all of the factors that influence the coating integrity:
- the composition of the coating
- the application/curing of the coating
- the quality of the surface being coated
When these are controlled, and the process is not merely validated in the research laboratory, but production-level verification is done to ensure that risks are minimized, manufacturers can move forward with certainty that each device is coated properly.
How to Determine if a Medical Device is Properly Coated
Medical device manufacturers undergo an intensive process validation procedure when they set up a new production sequence to gain approval. One reason for this extensive pre-production process is to build a production flow that is so well designed that it inevitably results in products that fulfill all necessary requirements.
Even though that sounds absolutely wonderful, it is an arduous and expensive process. Manufacturers are always looking for ways to improve their production-level process controls that can verify the product at various stages of production. This is more than just performance testing; it is continuous process monitoring and quality control.
A difficulty for manufacturers is implementing process controls that correlate to non-destructive testing done in the development lab, which, in this case, preserves the device's sterility.
Fibrinogen Assay
This common test uses a radioactive compound in a solution in which tubes are submerged. Then, the amount of sites the radioactive compound sticks to is measured. This is essentially modeled after one of the ways that the body clots blood. Fibrinogen is produced by the liver and released into the bloodstream to cause coagulation. If you have a high count on the assay, it indicates a lot of clotting taking place, and the coating is not present enough or lubricious enough.
Contact Angle Measurements
A simple contact angle measurement can be used to determine the presence of a coating. Contact angles measure a surface's wettability, which is another way of saying how hydrophilic a surface is. Inconsistent contact angles over the entirety of a surface can indicate that the coating may not have been uniformly applied because when a drop of liquid is placed on the surface during the contact angle test, it should wet out consistently over the entire surface.
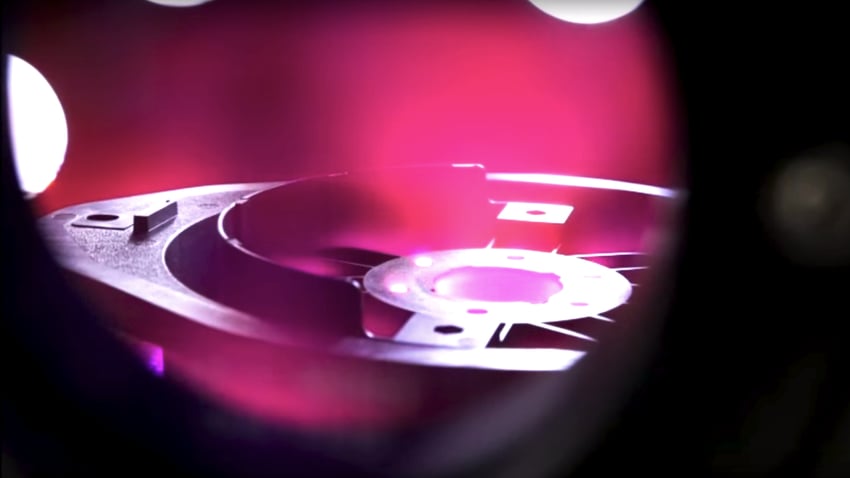
In research and development laboratories, contact angles are typically measured using a benchtop goniometer. A planar, smooth sample is placed on a stage, a drop of liquid is gently placed on the surface via a syringe, and the contact angle is measured from a side view of the sessile drop. Portable contact angle measurement devices have recently become available to make this validation method possible directly on actual devices being manufactured in both handheld and automated solutions. Because results are displayed quantitatively as an exact contact angle, there is no subjectivity, and the measurement correlates directly to predictable adhesion and cleanliness.
Since this is a legacy method that manufacturers are familiar with, contact angle measurements can be key in bridging the gap between the laboratory and the production line.
To get coatings to adhere to the surface of a device, the material needs to be cleaned, and the surface must be activated. Surface cleanliness, as it relates to coating adhesion, is the chemical compatibility between the material surface and the coating. To make the two more compatible, the surface is washed and treated to clean off residues and to make the surface reactive and ready to bond to the coating. With medical devices, there may be an aqueous wash process and/or a plasma treatment step to create a surface to which a coating will be highly attracted.
Contact angles measure surface quality before and after cleaning and treatment and track the changes that occur during those procedures. Measuring the bondability of the surfaces that come into contact with patients by getting a full picture of the entire surface is the best way to ensure a coating will reliably and uniformly adhere to the device.
Rethink your adhesion manufacturing processes with Surface Intelligence.
Lubricity Testing of Implantable Medical Devices
One of the most important characteristics of coatings on medical devices designed for use within the human body is the hydrophilic nature of that coating.
A hydrophilic coating will have an extremely low to no contact angle because liquids spread out completely on the surface and slide right off. This lubricious quality allows blood that comes into contact with tubing and devices protected by these coatings to flow (or wick) right over and around them without any impediments.
These coatings reduce friction, allowing for ease of insertion during surgeries and ensuring that they will not cause blood clotting around the device so it can remain in the body for the necessary length of time. Think of PICC lines used to administer chemotherapy and medications. These lines sometimes need to remain in the body for days or weeks, and they need to be unobtrusive during their stay.
Lubricious coatings prevent blood coagulation, so the tubing can remain in the body longer and does not need to be tended to or flushed as often.
Testing the frictional qualities of surfaces is extremely important to medical device manufacturers so they can ensure the comfort and safety of the end user, who is usually a patient. The amount of lubricity is called the coefficient of friction and can be measured by what is known as a pinch test.
In a pinch test, a coated device is pulled between the jaws of a clamp. While clamped, the coated part is pulled at a fixed speed for a fixed distance, and the resistance to the pull is measured in grams of pull force. A similar test, usually for films and flat materials, utilizes a plate that is slid over the surface of the material being tested. The grams of pull force needed to overcome the friction produced by the clamps divided by the clamping force is the calculation for the coefficient of friction (CoF). CoF = Forcepull/ Forceclamp. The higher the pull force needed, the higher the coefficient of friction and the lower the surface lubricity. The lower the pull force, the lower the coefficient of friction and the higher the lubricity.
Using contact angle measurements for coating inspection correlates well with coefficient of friction testing and could enhance or replace common testing methods. Clinical performance tests often involve using animals to understand the coatings' safety and effectiveness. Manufacturers are often looking for alternatives to these trials, and using a quality check like contact angle measurements could help decrease reliance on these tests.
Download our eBook to learn more about implementing verification tests into your production process, which makes scaling up from development easier. Medical device manufacturers have options for producing the most consistent and failure-free products. Download your copy of How to Streamline Process Design to Production for Medical Devices.